Eforto® for Healthcare Professionals
A New Vital Sign for Clinical Decision Making.
Eforto® supports clinical decisions, rehab and disease management with actionable biomarker insights.
Eforto® Supports Care Planning with Gold-Standard Metrics
Eforto®'s validated system for monitoring muscle health and vitality capacity is designed to provide actionable insights at multiple stages of the patient journey.1
From proactive prevention to chronic disease management, Eforto® offers objective data to guide personalized clinical decisions and improve outcomes.
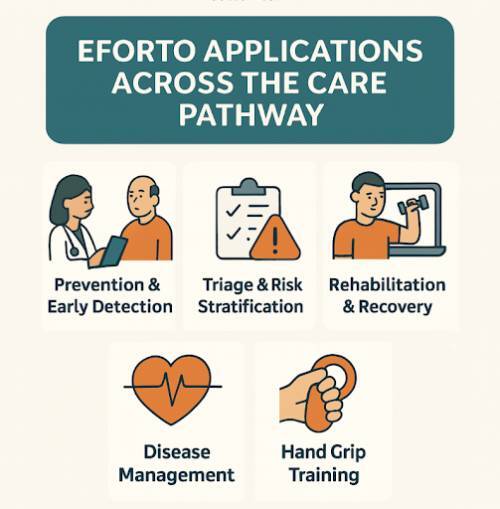
Eforto®: Solutions at Every Stage of Care
-
Prevention & Early Detection
In this phase, Eforto® is used as a proactive tool to identify risks before symptoms become severe, enabling timely and often reversible interventions.
A. Pre-frailty Screening: Eforto® functions as an early detection tool for pre-frailty, enabling intervention while the condition is still reversible. Continuous monitoring of vitality capacity and subtle changes in intrinsic capacity helps clinicians identify at-risk individuals before a formal frailty diagnosis, supporting healthy aging and independence.2
B. Intrinsic Capacity: Handgrip strength is strongly linked to multiple domains of intrinsic capacity—including mobility, cognition, psychological health, vitality, and sensory function. This makes it a powerful multi-dimensional biomarker of aging and an essential measure for frailty prevention and resilience assessment in older adults.3
C. Sarcopenia Case-Finding: Eforto® system addresses the unmet need for practical and sensitive tools for sarcopenia screening. It offers a more comprehensive functional assessment than simple questionnaires like the SARC-F, which often only identify more severe cases.4
D. Bone Health & Osteopenia: Low grip strength in individuals with reduced bone mass is a strong predictor of adverse outcomes. Routine monitoring with Eforto® provides a valuable strategy for managing osteopenia, helping to flag patients at higher risk and supporting timely interventions.5
E. Motor Function & Frailty: Motor function is the central link between sarcopenia, frailty, and adverse health outcomes. By quantifying both strength and fatigability, Eforto® enables clinicians to assess physical reserves with greater precision and guide interventions that maintain mobility and independence.6
F. Healthy Aging Monitoring: Eforto® supports the longitudinal tracking of vitality capacity, aligning with the WHO's model of healthy aging.7 allowing individuals and their health professionals to make timely lifestyle changes related to fitness and nutrition. Early identification of mobility and strength impairments through these assessments can help target interventions to reduce healthcare costs in aging populations. 8 -
Triage & Risk Stratification
Eforto® provides objective data to assess a patient's physical resilience, helping clinicians stratify risk and make informed decisions about the intensity and type of care needed.
A. Pre-Surgical Assessment: It can be used to establish a pre-operative baseline of a patient's functional capacity. This helps identify high-risk individuals who may benefit from prehabilitation to better withstand the physiological stress of surgery.9
B. Discharge Optimization: The system provides objective indicators of a patient's physical reserves, which can support safer and more confident hospital discharge decisions.10 -
Rehabilitation & Recovery
Eforto® offers a quantitative and objective method to track progress during recovery from an acute event, enabling personalized and data-driven rehabilitation.
A. Post-Surgical and Post-Event Monitoring: It is used to monitor recovery after a health stressor like major surgery (e.g., hip surgery), illness, or long COVID. This is a core target application for the Eforto® system. Objective muscle strength assessment is a reliable method for evaluating both upper and lower extremities in post-stroke patients with chronic hemiparesis. 11,12
B. Remote Rehabilitation: The system is ideal for telerehabilitation, providing objective, remote tracking of functional recovery. This helps overcome access barriers and allows therapists to monitor progress between clinic visits. 13C. Tracking Intervention Effectiveness: Muscle fatigability, measured by Eforto®, is a sensitive marker for tracking a patient's response to interventions like physical therapy or anti-inflammatory treatments. 14,15
-
Disease Management
For patients with chronic conditions, Eforto serves as a tool for longitudinal monitoring, helping to manage the disease's impact on physical function and evaluate treatment efficacy.
A. Chronic Condition Monitoring: Eforto® can be used to monitor the effectiveness of medication, nutrition, physical therapy, and coaching for patients with chronic diseases.
B. Neuromuscular Disease Progression: In conditions like ALS, Eforto® can track changes in muscle function, offering insights into disease progression and the effectiveness of therapy. 16C. Assessing Frailty in Chronic Illness: The system is applicable for monitoring frailty and muscle health in patients with chronic conditions such as COPD, kidney disease, and post-COVID syndrome. 17
-
Hand Grip Training
Beyond assessment, Eforto® serves as an interactive training tool that uses real-time biofeedback to make strengthening exercises more engaging and effective for both healthy aging and rehabilitation form from stroke, surgery, or injury.
A. Biofeedback for Guided Rehabilitation: The Eforto® training game provides real-time visual feedback based on each patient’s maximal grip strength, helping stroke, surgery, or injury patients perform exercises correctly and improve motor control. This sensor-based system makes hand rehabilitation more engaging. Additionally, resistance training can enhance muscle strength and VO₂ peak in HFrEF patients and should be integrated into both center- and home-based rehabilitation. 18,19
B. Gamified Training for Engagement: Eforto® transforms repetitive grip strength training into a motivating experience. An integrated game challenges users to meet goals and beat previous scores, improving adherence to training protocols for older adults combating sarcopenia and for athletes seeking to enhance performance.
C. Closed-Loop System: By combining training with assessment, Eforto® creates a powerful feedback loop. Users and their clinicians can immediately see the results of their training efforts, providing positive reinforcement and enabling data-driven adjustments to their exercise programs.
Empowering Clinical Practice Through Comprehensive & Multidisciplinary Care
The Eforto® M1 Vigorimeter is a medical device designed to provide rapid, reliable data on patient strength, endurance, and physical reserves that Integrate objective, validated biomarkers of muscle health and vitality into your clinical workflow.
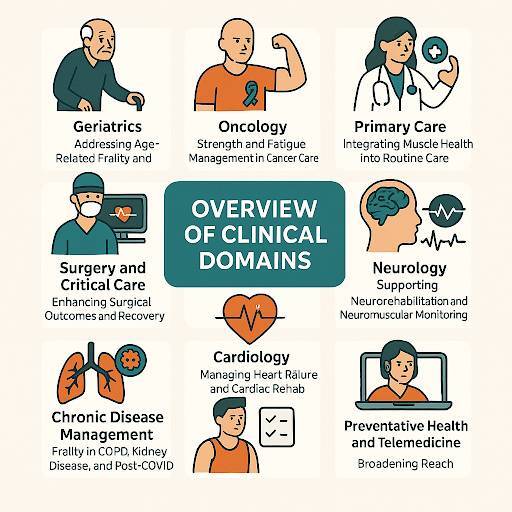
Eforto® Applications by Speciality Practice
-
Geriatrics
Addressing Age-Related Frailty and Decline
The challenge of managing frailty and sarcopenia is central to geriatric medicine. Early identification and intervention are key to preserving independence and improving quality of life for older adults (Epidemiology—Frailty Science).
Relevance: Grip strength is a core component of the frailty phenotype, and declining muscle function is a hallmark of sarcopenia.20 Early detection is critical, as older adults with the lowest grip strength have a 41% higher risk of all-cause mortality and a 63% higher risk of cardiovascular death compared to those with the highest strength.21
Strength decay during sustained maximal handgrip varies by age and clinical condition, with older adults showing particularly rapid decline early in the effort.22 Fatigability on the other hand serves as a sensitive prognostic marker of phenotypic aging, offering insight into how fatigue contributes to functional decline and the disablement pathway.23
Application: Eforto® offers a 5-minute standardized test that can be easily integrated into annual wellness visits or geriatric assessments. It quantifies maximal grip strength and, uniquely, muscle fatigability, providing a more sensitive indicator of declining physical reserves than strength alone.
Clinical Impact: By identifying patients with low or declining muscle function, Eforto® enables timely interventions such as physical therapy, nutritional counseling, and falls prevention programs. Its remote monitoring capabilities also allow tracking of post-hospitalization recovery, helping to mitigate functional decline.24
-
Oncology
Strength and Fatigue Management in Cancer Care
Cancer and its treatments frequently lead to debilitating side effects, including cancer cachexia (muscle wasting) and severe cancer-related fatigue (CRF). Managing these conditions is critical for maintaining treatment tolerance and patient quality of life.
Relevance: Involuntary muscle loss affects 50–80% of patients with advanced cancer and is a direct contributor to mortality.25 Cancer-related fatigue is one of the most common and distressing symptoms, impacting 70–90% of patients undergoing treatment. 26
In cancer survivors, fatigability serves as a sensitive, “hidden” biomarker—often outperforming muscle strength in predicting endurance loss and functional vulnerability.27
Application: Eforto® provides an objective tool to monitor muscle function throughout the cancer journey. Regular assessments can detect the early onset of cachexia by tracking declines in strength and endurance, prompting earlier nutritional or rehabilitative support. For CRF, Eforto® distinguishes physical fatigability from subjective tiredness, helping to tailor interventions and validate the patient's experience.
Clinical Impact: Proactive monitoring with Eforto® helps maintain a patient's strength, which can improve their ability to complete planned chemotherapy cycles and tolerate treatment. In survivorship, it serves as a motivational tool to track functional recovery and guide rehabilitation for the millions of cancer survivors worldwide.28 -
Primary Care
Integrating Muscle Health into Routine Care
Primary care is the frontline of preventive medicine. Integrating a quick, objective measure of muscle health and frailty can shift the focus from reactive treatment to proactive health management for aging adults.
Relevance: Grip strength is a powerful predictor of future morbidity, hospitalization, and all-cause mortality.29 It serves as a simple yet effective “vital sign” for overall physiological resilience, providing primary care clinicians with a practical tool to assess patient health.
Fatigue, a common and multidimensional challenge in primary care, is closely linked to grip strength, with individuals exhibiting low strength facing approximately a 30% higher risk of short-term hospital readmission or critical care.30,31
Application: The 5-minute Eforto® test can be seamlessly incorporated into annual physicals or wellness clinic visits. A low or declining score on grip strength or muscle endurance can trigger further investigation or referrals for preventive care, such as nutrition counseling or physical therapy.
Clinical Impact: Eforto® empowers primary care providers to identify at-risk individuals early, long before functional decline becomes apparent. This creates opportunities for preventive interventions that can delay the onset of frailty, manage chronic conditions more effectively, and reduce downstream healthcare costs. -
Surgery and Critical Care
Enhancing Surgical Outcomes and Recovery
A patient's physical reserve is a critical determinant of their ability to withstand the stress of major surgery or critical illness. Assessing frailty preoperatively and tracking recovery postoperatively are key to improving outcomes.
Relevance: Frailty significantly increases the risk of postoperative complications, longer hospital stays, and mortality.
Patients with high frailty scores are 2.8 times more likely to experience complications and 32 times more likely to die compared to non-frail patients.³² ICU-acquired weakness affects 25–31% of critically ill patients, rising to 25–50% in those with prolonged ICU stays and up to 70% among elderly ICU patients, representing a major contributor to long-term disability.33
Preoperative low handgrip strength is linked to approximately 2.2 times higher odds of postoperative complications.34 In one surgical cohort, major complications occurred in 40.3% of patients with low handgrip strength versus 24.6% of those with high strength.35 Surgery-induced inflammation further reduces muscle endurance and increases fatigue, with elderly patients being particularly affected.⁹
Beyond surgery, handgrip strength in community-dwelling older adults predicts subsequent declines in cognition, mobility, functional ability, and overall risk of mortality.36
Application: Eforto® can be used in pre-surgical clinics as a rapid screening tool for frailty, identifying high-risk patients who would benefit from prehabilitation. Post-operatively or after an ICU stay, it enables remote monitoring of a patient's strength and endurance recovery thanks to its ergonomic design, providing a quantitative trajectory that can alert clinicians to setbacks or suboptimal progress.
Clinical Impact: Integrating Eforto® into the perioperative pathway facilitates data-driven decisions. It helps optimize patients for surgery through targeted prehab, supports safer discharge planning, and allows for timely intervention if post-discharge recovery falters, ultimately reducing complications and readmissions. -
Cardiology
Managing Heart Failure and Cardiac Rehab
Heart failure is a systemic condition where muscle weakness and frailty are highly prevalent and are strong predictors of poor outcomes.
Relevance: Approximately 50% of heart failure patients are frail, which significantly increases their risk of hospitalization and mortality.37 Lower relative grip strength is associated with an approximately 21% higher risk of cardiovascular disease.38 In addition, perceived fatigability rises with higher cardiovascular risk, particularly among individuals with hypertension, highlighting that promoting screening for these biomarkers can also help control these conditions, especially in adults under 70.39
Application: In heart failure clinics, Eforto® provides a quick, objective measure of frailty status, helping to stratify risk and guide therapeutic decisions. As part of a remote patient monitoring (RPM) program, a decline in grip strength can act as an early warning sign of clinical decompensation. For cardiac rehabilitation, Eforto® tracks improvements in muscle endurance, providing objective feedback that can enhance patient motivation and adherence, addressing the challenge that only 20-30% of eligible patients enroll in these vital programs.40
Clinical Impact: By making frailty a measurable vital sign in cardiology, Eforto® helps personalize care for high-risk heart failure patients. It enhances the effectiveness of cardiac rehabilitation and provides a new data stream for remote monitoring programs, contributing to reduced hospitalizations and improved functional capacity. That’s why Grip strength can serve as a simple, low-cost risk screening tool for ambulatory clinics, eliminating the need for imaging and avoiding the limitations of walking-based measures. 41 -
Neurology
Supporting Neurorehabilitation and Neuromuscular Monitoring
Neurological conditions are often characterized by progressive weakness and significant fatigue. Objective, frequent measurement is essential for tracking disease progression, titrating therapies, and guiding rehabilitation.
Relevance: Conditions such as stroke, Multiple Sclerosis (MS), ALS, and Myasthenia Gravis (MG) involve impaired neuromuscular function that can fluctuate over time, requiring continuous monitoring. Fatigue is a prevalent and complex symptom in these disorders, with multiple underlying causes. Neurophysiological testing provides an objective, cost-effective biomarker to identify the origin of fatigue, evaluate its severity, and guide personalized treatment and rehabilitation strategies.42
Application: Eforto® serves as a versatile tool across neurological rehabilitation. In stroke rehabilitation, it quantifies motor recovery in the affected limb and provides motivating feedback for patients, supporting the care of the estimated 93.8 million global stroke survivors.43 Stroke remains a leading cause of death worldwide, with lifestyle factors contributing to increased risk.44
For patients with immune-mediated neuropathies such as GBS and CIDP, grip strength assessment using the Vigorimeter is preferred. 45 In Multiple Sclerosis (MS), Eforto® offers an objective measure of physical fatigability to complement subjective reports and guide energy management strategies.
Clinical Impact: Eforto® enables data-driven neuromuscular assessment, offering objective trial endpoints, personalized rehabilitation, and quantitative insights for disease management. In ALS, frequent home monitoring improves tracking of functional decline, while in MS, higher handgrip strength correlates with better function, balance, and quality of life—supporting routine HGS measurement in care. 46 -
Chronic Disease Management
Frailty as a Key Biomarker in Chronic Diseases
Systemic inflammation and catabolism in many chronic diseases accelerate muscle loss and frailty, worsening prognosis and quality of life.
Relevance: Muscle weakness is a key comorbidity in COPD, chronic kidney disease (CKD), and a persistent symptom in many individuals with Post-COVID Syndrome, limiting exercise capacity and increasing mortality risk. Clinically significant fatigue is highly prevalent in COPD and correlates with greater disease burden, making it an important marker for prognosis and disease management.47
In CKD patients, low grip strength is associated with an approximately 96% higher risk of all-cause mortality.48 Similarly, in older adults with type 2 diabetes and other comorbidities, low grip strength is linked to about 56% higher risk of hospitalization over follow-up.49
Application: Eforto® offers a simple, non-exertional way to monitor systemic muscle health in patients who cannot perform traditional exercise tests. It can track the impact of pulmonary rehabilitation, monitor the effects of dialysis on muscle endurance in CKD, and quantify functional recovery in Post-COVID patients.
Clinical Impact: By providing a reliable proxy for overall muscle health, Eforto® helps clinicians manage the systemic effects of chronic diseases, assess the efficacy of interventions, and objectively track a patient’s functional status over time. -
Occupational Health
Enhancing Workplace Safety and Recovery
In physically demanding industries, managing employee fatigue is crucial for preventing costly injuries and ensuring a safe work environment.
Relevance: Grip strength and muscle endurance are objective indicators of an employee’s physical readiness. A significant decline in performance can signal fatigue risk, which is a major contributor to workplace accidents. Workers with low grip strength have an approximately 20% higher probability of future work limitations.50
Fatigue is also strongly associated with both short- and long-term sickness absence, making it a reliable predictor of workplace absenteeism. Screening tools such as the Checklist Individual Strength can help identify employees at risk and inform preventive interventions.51
Application: Eforto® can be utilized for pre-employment baseline testing to ensure candidates meet the physical demands of a role. It also functions as a tool to monitor fatigue during shifts and to objectively track functional recovery after a workplace injury, supporting evidence-based return-to-work decisions.
Operational Impact: Eforto® provides occupational health managers with a simple, quantitative screening tool to mitigate injury risk, manage employee fatigue proactively, and create safer and more productive work protocols. -
Sports Medicine
Optimizing Performance and Recovery
For athletes and athletic programs, the margin between peak performance and overtraining is narrow. Managing training loads and recovery is essential for preventing injuries and achieving competitive goals.
Relevance: Grip strength and muscle endurance are reliable markers of neuromuscular readiness and CNS fatigue, with declines signaling overtraining risk before performance drops. In some athlete cohorts, lower preseason grip strength correlates with higher odds of decline or injury, with injury incidence around 25% in sport-specific studies.52
Monitoring these measures helps prevent overtraining, illness, and injury while providing actionable feedback to optimize training and communication. Handgrip strength training can enhance performance in hand-intensive sports, though outcomes also depend on technique, physical capacity, body composition, and tactics. Collaboration among sport scientists and coaches is key to maximizing results.53,54
Application: Eforto® can be used as a daily "readiness-to-perform" check for athletes. The objective data helps coaches and trainers make informed decisions to guide daily training loads, ensuring athletes are pushed optimally without being pushed into a state of overtraining.
Performance Impact: Eforto® equips coaches, trainers, and sports medicine professionals with a simple, quantitative tool to personalize training, mitigate injury risk, and ensure athletes are physiologically ready for peak performance. -
Longevity Clinics
Quantifying Physical Resilience for Healthy Aging
Regular assessment of muscle strength and endurance provides clinicians with actionable biomarkers to detect early functional decline. Tracking these metrics allows for timely, personalized interventions that support resilience and maintain independence in older adults.
Relevance: Longevity clinics focus on optimizing biological age and functional capacity across the lifespan. Frailty and sarcopenia are major accelerators of biological aging and can undermine the benefits of precision medicine and anti-aging interventions since Lower handgrip strength predicts longer hospital stays and poorer physical quality of life, making it a valuable tool to identify frailty and guide early interventions during hospitalization.55
Fatigability also is a powerful prognostic marker of phenotypic aging, offering early insight into how fatigue contributes to the progression of functional decline.56
Application: Eforto® enables routine, longitudinal tracking of muscle strength and endurance—two hallmarks of physical vitality. By integrating Eforto® into biological age assessments, clinics can establish a personalized functional baseline and monitor the effects of interventions such as hormone therapy, exercise regimens, or nutraceuticals.
Clinical Impact: Objective muscle performance data adds a new dimension to biological age scoring systems, providing actionable insight into physical reserve. Over time, Eforto® can demonstrate the effectiveness of interventions in reversing or slowing down functional decline, empowering patients with feedback and motivating adherence to healthy aging strategies. -
Fatigue and Chronic Fatigue Clinics
Disentangling Physical from Perceived Fatigue
Objective assessment of muscle fatigability offers clinicians a reliable biomarker to detect early functional decline that may not be apparent through patient reports alone. Monitoring these metrics over time enables personalized intervention planning and more effective management of chronic fatigue conditions.
Relevance: Chronic fatigue conditions, including Myalgic Encephalomyelitis/ Chronic Fatigue Syndrome (ME/CFS), long COVID, and fibromyalgia, are marked by debilitating fatigue that may not be detectable with conventional tests. Differentiating between physical fatigability and subjective tiredness is a critical challenge, with fatigability often revealing functional decline earlier than maximal strength.57
Functional Assessment: In patients with chronic fatigue, handgrip strength correlates with and predicts maximal exercise capacity, making it a simple, objective, and practical measure of functional performance.58
Application: Eforto® provides a unique capability to measure muscle fatigability objectively, distinguishing it from self-reported symptoms. Clinicians can track changes over time and assess treatment responses—whether through graded activity, pacing, pharmacologic interventions, or lifestyle modifications—using standardized, reproducible metrics.
Clinical Impact: By quantifying the physiological component of fatigue, Eforto® supports more precise diagnosis and targeted interventions. It also provides validation to patients whose symptoms are often misunderstood or minimized, enhancing therapeutic alliance and enabling personalized rehabilitation strategies. -
In-Pharmacy Screening
Early Detection of (Sub)Clinical Frailty
Early identification of declining muscle strength and fatigability allows pharmacists to act as frontline detectors of (sub)clinical frailty. These assessments provide actionable insights that can guide referrals, lifestyle recommendations, or adjustments in medication management.
Relevance: Pharmacies are increasingly becoming community health hubs, well-positioned to detect early signs of health deterioration. Frailty often develops silently and is only recognized after adverse events like falls, hospitalizations, or rapid functional decline. Fraility is associated with increased adverse outcomes and may predict higher risk of drug toxicity or complications, e.g., in chemo or polypharmacy contexts. 59
Application: With its 5-minute protocol and portable device, Eforto® is ideal for pharmacy-based screening programs. Pharmacists can integrate muscle function assessments into medication reviews or wellness campaigns, identifying individuals with low strength or high fatigability who may benefit from early intervention or referral.
Public Health Impact: By making frailty screening more accessible, Eforto® empowers pharmacies to play a key role in preventative care. Early detection of declining muscle health enables timely lifestyle or medical interventions, helping to reduce the burden of avoidable hospitalizations and preserve independence among aging adults. -
Nutrition & Dietetics
Strengthening Capacity for Better Quality of Life
Maintaining adequate nutrition is a cornerstone of muscle health, functional performance, and overall well-being. Early detection of nutritional deficits allows for timely interventions that preserve strength, prevent frailty, and improve clinical outcomes.
Relevence: Malnutrition, sarcopenia, and frailty are common but often overlooked conditions that can lead to serious health problems. Grip strength is a key indicator of nutritional status and physical capacity in older adults, with declines signaling frailty, increased malnutrition risk, cachexia, and reduced function. In malnourished surgical or oncology patients, low handgrip strength is associated with roughly twice the risk of complications or mortality and longer hospital stays.60
Handgrip strength also reflects early changes in muscle function due to nutritional deprivation and is widely used to assess nutritional status and evaluate outcomes in intervention studies.61 Additionally, poor diet quality is linked to higher perceived physical fatigability, which explains about 65% of the association with reduced physical function.62
Application: Eforto® empowers dietitians with objective, real-time data on muscle function, enabling tailored nutrition plans based on each patient’s physical reserves. Its mobile platform supports continuous monitoring of nutritional outcomes, ensuring early intervention, treatment tracking and personalized care in both remote and in-person settings.
Public Health Impact: Eforto® enables widespread screening for malnutrition and muscle loss, allowing early dietary interventions. This helps reduce hospital stays, supports recovery, and promotes healthier aging across populations. -
Remote Patient Monitoring
Broadening Reach and Continuity of Care
The future of healthcare is proactive and decentralized. Eforto® supports scalable preventive care and telehealth by enabling patients to track muscle function and fatigability at home. This empowers self-management, while early detection of declining reserves allows timely interventions, improving outcomes and reducing costs.
Relevance: Effective telemedicine and remote patient monitoring (RPM) require objective, reliable data that can be collected by patients at home. Eforto® enables clinicians to capture precise measures of muscle strength and fatigability remotely, which are critical indicators of functional capacity and overall health status. These metrics help identify early signs of decline, track chronic disease progression, and support proactive interventions, ensuring care is data-driven even outside clinical settings.13-15
Application: Eforto®’s self-guided mobile app combined with the validated vigorimeter is ideal for telehealth and RPM programs targeting healthy aging, chronic disease management, or post-discharge rehabilitation. The system supports remote rehabilitation by allowing therapists and health coaches to objectively monitor patients’ functional recovery between visits, overcoming access barriers and maintaining continuity of care. Muscle fatigability, measured through Eforto®, also serves as a sensitive marker for evaluating patient responses to interventions such as physical therapy, anti-inflammatory treatments, or tailored exercise programs.
Clinical Impact: By extending the reach of clinicians beyond the hospital walls, Eforto® enables scalable and cost-effective monitoring of at-risk populations. Real-time data on strength and endurance empowers health coaches and care managers to detect negative trends early, initiate timely interventions, and adjust care plans based on objective feedback. This approach facilitates preventive care, enhances patient independence, reduces readmissions, and ultimately supports healthier outcomes for individuals managing chronic conditions or recovering from acute health events.
“Growing older doesn’t have to mean growing weaker. With Eforto®, your energy becomes something you can understand — and improve."

Vrije Universiteit Brussel (VUB), BelgiumChair,
WHO Working Group on Vitality Capacity
"With Eforto® tracking muscle health and vitality capacity become as easy as measuring blood pressure. It should be part of every routine checkup."

-
List of References:
-
Vaishya R, Misra A, Vaish A, Ursino N, D’Ambrosi R. Hand grip strength as a proposed new vital sign of health: a narrative review. J Health Popul Nutr. 2024;43:7.
-
Knoop V, Costenoble A, Debain A, et al. Interrelationship between grip work, self-perceived fatigue, and pre-frailty in octogenarians. Exp Gerontol. 2021;152:111440.
-
Arokiasamy P, Selvamani Y, Jotheeswaran AT, Sadana R. Socioeconomic differences in handgrip strength among older adults. Sci Rep. 2021;11:19494.
-
Sipers WM, Verdijk LB, Sipers SJ, Schols JM, van Loon LJ. Martin vigorimeter vs Jamar dynamometer in geriatric patients. J Am Med Dir Assoc. 2016;17:466.e1.
-
Sun H, Liu J, Tan R, et al. Hand grip strength and all-cause mortality in decreased bone mass: NHANES study. Front Med. 2024;11:1452811.
-
Buchman AS, Leurgans SE, Wang T, et al. Motor function drives associations of sarcopenia and frailty with adverse outcomes. PLoS One. 2021;16:e0245680.
-
Bautmans I, Knoop V, Thiyagarajan JA, et al. WHO working definition of vitality capacity. Lancet Healthy Longev. 2022;3:e789-e796.
-
Avlund K. Fatigue in older adults: an early indicator of aging? Aging Clin Exp Res. 2010;22:100-115.
-
Bautmans I, Njemini R, De Backer J, De Waele E, Mets T. Surgery-induced inflammation, age, muscle endurance, and fatigue. J Gerontol A Biol Sci Med Sci. 2010;65:266-273.
-
Arnold P, Njemini R, Vantieghem S, et al. Peripheral muscle fatigue in hospitalized geriatric patients. Exp Gerontol. 2017;95:128-135.
-
De Lorenzo R, Di Filippo L, Scelfo S, et al. Longitudinal changes in physical function in COVID-19 patients. Nutrients. 2023;15:4474.
-
Rabelo M, Nunes GS, da Costa Amante NM, de Noronha M, Fachin-Martins E. Reliability of muscle strength in chronic post-stroke hemiparesis. Top Stroke Rehabil. 2016;23:26-35.
-
Nicolas B, Leblong E, Fraudet B, et al. Telerehabilitation solutions: overview of systematic reviews. Digit Health. 2024;10:20552076241294110.
-
Mets T, Bautmans I, Njemini R, Lambert M, Demanet C. Celecoxib and muscle fatigue resistance in elderly. Am J Geriatr Pharmacother. 2004;2:230-238.
-
Beyer I, Bautmans I, Njemini R, et al. NSAID treatment vs placebo in geriatric patients with acute infection. BMC Musculoskelet Disord. 2011;12:292.
-
McGrath R, Johnson N, Klawitter L, et al. Association patterns between handgrip strength and adverse health conditions. SAGE Open Med. 2020;8:2050312120910358.
-
Azhimamatova R, Salieva RS, Zalova TB, et al. Frailty in COPD: Clinical impact, diagnosis, biomarkers, and management. Int J Chron Obstruct Pulmon Dis. 2025;2445-2458.
-
Sai Krishna MC, Monesh Karthikkeyan BA, Nair BB, Rajagopalan T. Sensor-based grip strength monitoring for stroke rehab. Adv Electr Comput Technol. 2020;789-802.
-
Ruku DM, TH TT, Chen HM. Center-based vs home-based resistance training in HFrEF: systematic review. Enfermeria Clin (Engl Ed). 2021:S1130-8621.
-
Yuan S, Larsson SC. Epidemiology of sarcopenia: prevalence, risk factors, and consequences. Metabolism. 2023;144:155533.
-
Wu Y, Wang W, Liu T, Zhang D. Grip strength and risk of mortality, CVD, and cancer: meta-analysis. J Am Med Dir Assoc. 2017;18:551.e17.
-
De Dobbeleer L, Beyer I, Njemini R, et al. Force-time characteristics during sustained maximal handgrip. Exp Gerontol. 2017;98:192-198.
-
Schrack JA, Simonsick EM, Glynn NW. Fatigability: a prognostic indicator of phenotypic aging. J Gerontol A Biol Sci Med Sci. 2020;75:e63-e66.
-
Van Grootven B, Jeuris A, Jonckers M, et al. Predicting hospitalization-associated functional decline in older cardiac patients. BMC Geriatr. 2020;20:112.
-
von Haehling S, Anker SD. Cachexia: prevalence, incidence, and clinical impact. J Cachexia Sarcopenia Muscle. 2014;5:261-263.
-
Poort H, Peters MEWJ, Van Der Graaf WTA, et al. CBT or graded exercise vs usual care for fatigue in advanced cancer. Ann Oncol. 2020;31:115-122.
-
Gresham G, Dy SM, Zipunnikov V, et al. Fatigability and endurance in cancer survivors: Baltimore Longitudinal Study. Cancer. 2018;124:1279-1287.
-
Li J. Nurses’ healthcare guidance for stroke rehabilitation: literature review. 2022.
-
Bohannon RW. Grip strength: an indispensable biomarker for older adults. Clin Interv Aging. 2019;1681-1691.
-
Connolly D, O’Toole L, Redmond P, Smith SM. Managing fatigue in patients with chronic conditions in primary care. Fam Pract. 2013;30:123-124.
-
de Melo TA, Guimarães FS, Silva JRLE. Gait speed, muscle strength, and functional status predict 30-day unplanned hospital readmission. Physiother Res Int. 2023;28:e2001.
-
Tse W, Dittman JM, Lavingia K, Wolfe L, Amendola MF. Frailty index and postoperative complications after lower extremity amputation. J Vasc Surg. 2021;74:963-971.
-
Wang W, Xu C, Ma X, et al. ICU-acquired weakness: review of recent progress. Front Med. 2020;7:559789.
-
Jiang X, Xu X, Ding L, et al. Preoperative handgrip strength and postoperative outcomes in GI tumors: systematic review. Support Care Cancer. 2022;30:6451-6462.
-
Li C, Chen Y, Wu H, et al. Handgrip strength and postoperative outcomes in primary liver cancer. Nutr Hosp. 2025;42.
-
Rijk JM, Roos PR, Deckx L, van den Akker M, Buntinx F. Prognostic value of handgrip strength in ≥60 years: systematic review. Geriatr Gerontol Int. 2016;16:5-20.
-
McDonagh J, Ferguson C, Hilmer SN, et al. Expert opinion on frailty management in heart failure. Heart Lung Circ. 2025.
-
Lopez-Bueno R, Andersen LL, Koyanagi A, et al. Handgrip strength thresholds for mortality: systematic review. Ageing Res Rev. 2022;82:101778.
-
Qiao Y, Martinez-Amezcua P, Wanigatunga AA, et al. Cardiovascular risk and perceived fatigability in mid-to-late life. J Am Heart Assoc. 2019;8:e013049.
-
Ades PA, Keteyian SJ, Wright JS, et al. Increasing cardiac rehab participation: Million Hearts roadmap. Mayo Clin Proc. 2017;92:234-242.
-
Reeve IV TE, Ur R, Craven TE, et al. Grip strength for frailty in vascular disease: comorbidity, cardiac risk, sarcopenia. J Vasc Surg. 2018;67:1512-1520.
-
Tankisi H, Versace V, Kuppuswamy A, Cole J. Clinical neurophysiology in fatigue and fatigability. Clin Neurophysiol Pract. 2024;9:39-50.
-
Feigin VL, Brainin M, Norrving B, et al. World Stroke Organization: Global Stroke Fact Sheet 2025. Int J Stroke. 2025;20:132-144.
-
Draak TH, Pruppers MH, Van Nes SI, et al. Grip strength in immune-mediated neuropathies: Vigorimeter vs Jamar. J Peripher Nerv Syst. 2015;20:269-276.
-
Seferoğlu M, Aksoy MK, Tunç A. Hand grip strength as predictive tool in MS. Int J MS Care. 2024;26:134-139.
-
Antoniu SA, Petrescu E, Stanescu R, et al. Impact of fatigue in COPD patients: exploratory study. Ther Adv Respir Dis. 2016;10:26-33.
-
Suliman ME, Ryu K, Qureshi AR, et al. Handgrip strength and mortality in kidney failure: normalization methods. Nutrition. 2024;125:112470.
-
Hamasaki H, Kawashima Y, Katsuyama H, et al. Handgrip strength with hospitalization, CV events, and mortality in T2DM. Sci Rep. 2017;7:7041.
-
Morera Á, Calatayud J, Casana J, et al. Handgrip strength and work limitations: cohort of adults ≥50. Maturitas. 2023;177:107798.
-
Janssen N, Kant IJ, Swaen GMH, et al. Fatigue as predictor of sickness absence: Maastricht cohort. Occup Environ Med. 2003;60:i71-i76.
-
Erickson BJ, Buchheit P, Rauch J, et al. Grip strength and injuries in professional baseball. Orthop J Sports Med. 2024;12:23259671241257622.
-
Halson SL. Monitoring training load to understand fatigue in athletes. Sports Med. 2014;44(Suppl 2):139-147.
-
Cronin J, Lawton T, Harris N, Kilding A, McMaster D. Handgrip strength and sport performance: brief review. J Strength Cond Res. 2017;31:3187-3214.
-
McNicholl T, Curtis L, Dubin JA, et al. Handgrip strength predicts length of stay and QoL. Clin Nutr. 2020;39:2501-2509.
-
Peeters, G., Swart, M.M., De Dobbeleer, L., Bautmans, I., Olde Rikkert, M.G. and Melis, R.J., 2025. Understanding hand grip measures in geriatric inpatients: associations with frailty, daily functioning and fatigue. Aging Clinical and Experimental Research, 37(1), p.293.
-
Jammes Y, Stavris C, Charpin C, et al. Maximal handgrip predicts maximal physical performance in chronic fatigue. Clin Biomech. 2020;73:162-165.
-
da Rocha IMG, Marcadenti A, de Medeiros GOC, et al. Cachexia and chemotherapy toxicities in GI cancer patients. J Cachexia Sarcopenia Muscle. 2019;10:445-454.
-
Xie T, Li J, Wu X, et al. Preoperative muscle function as predictor of postoperative outcomes in colorectal cancer with malnutrition. Front Nutr. 2025;12:1559111.
-
Norman K, Stobäus N, Gonzalez MC, Schulzke JD, Pirlich M. Hand grip strength: outcome predictor and nutritional marker. Clin Nutr. 2011;30:135-142.
-
Davis B, Liu YH, Stampley J, et al. Poor diet quality, physical fatigability, and function in oldest-old. Geriatrics. 2021;6:41.
-
Ready to Achieve Clinical Excellence with Eforto®?
Equip Your Care Team with Validated Vitality Monitoring
Discover how Eforto® can support early identification, monitoring, and personalized interventions across specialties. Find the right tools for your medical practice or research protocol.